View as pdf
A later version of this article appeared in Nurse Leader, Volume 21, Issue 6, December 2023.
Abstract
Recruitment and retention of strong nurse leaders is essential to our healthcare delivery system, highlighting a need for early career engagement and mentorship. Combining experiential and didactic learning through an academic-practice partnership facilitated the creation of a 1-year leadership program for pre-licensure nursing students, highlighting nursing leadership as a future career specialty. The Young Nurse Leader program combined educational sessions, precepted experiences, and self-reflection to enhance student nurses’ leadership knowledge and skills, while providing professional enrichment of the practicing nurse leaders who precepted, coached and mentored the students.
Nursing leaders face increased complexity, staffing turn over, high rates of change, work force shortages, and quality and safety issues, highlighting the need for workforce development.1,2 Furthermore, the COVID-19 pandemic exposed and highlighted inadequacies in the preparation and support of nurse managers. Nurse leaders, most notably nurse managers, are leaving their roles at alarming rates with 45% of nurse managers considering leaving their role.3 There is a critical need to retain and recruit nurse leaders with the appropriate knowledge, skills, and abilities to lead system redesign, re-engage the workforce, and implement sustainable interventions to deliver safe, high-quality care.3,4
The American Association of Colleges of Nursing’s (AACN) Essentials provided an outline for the necessary curriculum content and expected competencies for graduates of baccalaureate, master’s, and Doctor of Nursing Practice (DNP) programs.5 Establishing the expectations for the concept of leadership preparation in the AACN Essentials is the first step to reframing the role expectations and the need for leadership preparation for future nurses. To increase interest and knowledge growth of prospective nurse leaders, an opportunity to engage pre-licensure students in the development of leadership and management skills was identified. Academic-practice partnerships allow for a shared commitment of recruitment, retention, and leadership development while allowing exploration of leadership roles, identification of current strengths, and development of leadership skills.5,6 Additionally, supporting the development of a personal identity using educational environment to initiate mentoring, while concurrently having nursing leaders in the practice setting commit to role modeling nursing excellence, can foster nursing identity and role transitions.7,8
Developing a Nurse Leader
Leadership programs have been linked to increased self-awareness, enabling participants to recognize and acknowledge newly developing leadership behaviors and skills, which they had not imagined before.9 Additionally, participants voiced that they could feel the change occurring, sought out challenges for growth, and matured professionally and psychologically during the leadership program.9 Well-developed leadership skills have shown improved patient satisfaction and a reduction in adverse events, highlighting the direct benefits that leadership training has on direct patient care.9 Ongoing engagement in leadership development helps improve the nurse leaders’ abilities and can impact organizational performance. Identifying opportunities to provide threaded leadership knowledge and skill development can help promote seamless application of leadership skills to practice.10
Growing an Academic-Practice Partnership
In our academic medical center, high turnover, verbalized burnout, and a lack of interest in serving in nursing leadership roles, such as charge nurse, assistant nurse manager, or nurse manager became increasingly noticeable. Through informal discussion with nurse leaders, it became apparent that such roles did not spark interest for early career nurses, especially because of the lack of formal training or knowledge to serve in these roles. Therefore, if we want nurses to pursue early careers in nursing leadership, we must ensure that nurses possess the necessary leadership skills and competencies that will help them be successful leaders throughout their careers. The College of Nursing (CoN) has a rich history of providing undergraduate nursing students with additional professional development under the mentorship of faculty and expert clinicians. A popular specialty immersion program for undergraduates is called the Young Nurse Clinician Program, which provides experiential learning opportunities in geriatrics, pediatrics, psychiatry, palliative care, community health, and nursing education. However, a program emphasizing leadership growth and development did not exist. In a collaborative effort, an academic-practice partnership was formed to support the development of the Young Nurse Leader (YNL) program. The rich history of partnership that already existed between the academic medical center (AMC) and the CoN allowed growth of a program focused on engaging and enhancing the leadership focused training of pre-licensure students. Program Leaders (PL) included the CoN professor overseeing the masters and doctoral health systems tracks and the director of the medical-surgical services nursing division at the AMC.
YNL Program Development

The YNL program aimed to improve pre-licensure student awareness of and interest in leadership focused career paths, hone leadership knowledge and skills to promote seamless transition to practice, and meaningfully engage current nurse leaders in a shared opportunity to help prepare future nurse leaders. Pre-licensure students were selected, through an application process, to participate in the 1-year program which included didactic and experiential learning opportunities (Table 1). Throughout the year, students explored their interests in leadership and management career paths. PLs presented didactic content on relevant leadership topics monthly and then promoted peer discussion. For experiential learning, students were precepted by a practicing nurse leader who spent 4 hours with them monthly. Furthermore, students were encouraged to complete a project in collaboration with the PLs and/or their preceptor on a topic of interest to promote application of their developing leadership skills.
Didactic Curriculum
The annual curriculum topics are reviewed and finalized each year by the PLs. Topics are evaluated for continued relevancy to current practice challenges, as well as the importance from both an academic and practice standpoint. The monthly 1-hour didactic meetings provide the cohort with opportunities to learn from experts, ask questions, reflect upon their leadership experiences, and engage in meaningful discussion on a variety of topics. The collaborative environment of the program facilitated the exploration of leadership concepts, theories, and complex topics of interest to the students using real-world application. Changes were made to the topics each year and the current curriculum is found in appendix, table 2.
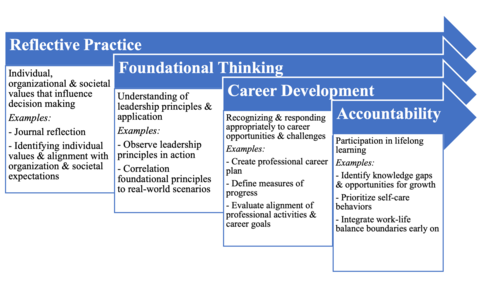
The YNL program emphasized the need for self-reflection, which is an important piece of the AACN Essentials5 and American Organization for Nursing Leadership (AONL) Nurse Leader Competencies (Figure 1).11 Participants were encouraged to partake in self-reflection to better understand the impact that their experiential learning had on their growth as a nurse leader. Through facilitated discussion, students were able to verbalize their leadership perspectives, observations, and personal experiences, all which shape who they are as aspiring nurse leaders.
Experiential Learning
Identifying nurse leaders who wanted to engage as a preceptor and mentor with a pre-licensure student occurred at the beginning of each academic year. Then YNL participants were paired with preceptors who shared similar interests and leadership goals. The preceptors agreed to spend 4 hours each month. Preceptor objectives included outlining the expectations and operations related to their formal leadership role, share their personal experiences and leadership journey, review unit or division level projects and initiatives lead by the preceptor, and provide real-world examples to be discussed during the monthly didactic sessions.
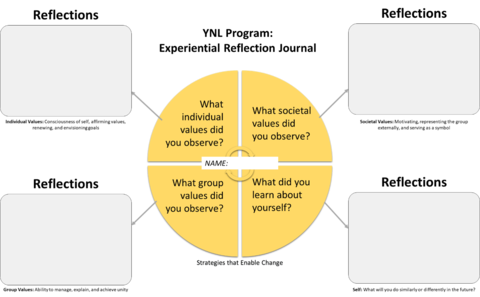
Students were asked to complete an experiential journal each month (Figure 2) based on the didactic topic and observations from their time with the preceptor. The journal format was inspired by the Leadership Development Model12 which highlights the importance of individual values, group values, and society values. This format helped facilitate a global reflection of the leadership experiences YNL participants had with their preceptors and provided a consistent format for student self-reflection during the monthly didactic meetings.
Results
Since beginning in 2020, the YNL program has accepted 8 aspiring leaders to participate in the program. All 8 participants completed the YNL program during their third or fourth year as an undergraduate student. The participants were paired with preceptors at the local academic medical center, with preceptor roles including nurse manager, assistant nurse manager, nursing practice leader, and nursing director. The preceptors practiced in a variety of areas, including medical-surgical services, intensive specialty services, behavioral health, and children and women services. Preceptors had between 5 and 30 years of nursing experience.
At the end of each academic year, survey links were emailed to YNL participants and preceptors with the request to provide feedback on their experience with the program. A 5-point Likert scale (strongly disagree to strongly agree) was used to assess satisfaction, value, and leadership growth. Additionally, open-ended questions sought feedback on strengths and opportunities within the program. Information from the surveys helped program leaders make necessary adjustments to enhance the experience for both students and preceptors and improve program quality.
Student Satisfaction
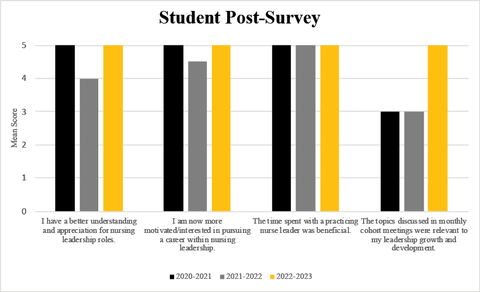
Five (62.5%) students completed a post-program survey (Figure 3). Students in Cohort 1 were highly satisfied with their preceptorship but provided feedback that the didactic sessions could be improved to better meet their learning needs. Cohort 2 experienced significant disruptions related to a COVID-19 surge that negatively impacted hospital leadership availability and access. During this surge, multiple didactic sessions were cancelled to accommodate for the significant impact and resource demand within the academic medical center. Cohort 3 was able to meet in-person after COVID-19 restrictions had been relaxed, and leaders were able to engage with YNL participants throughout the year. As expected, student survey data decreased during Cohort 2 but increased in Cohort 3 when operations normalized. Students shared that the preceptorship with a nurse leader and monthly cohort discussions were their favorite aspects of the program. 100% of students who completed the survey said that they would recommend the YNL program to other students.
Preceptor Satisfaction
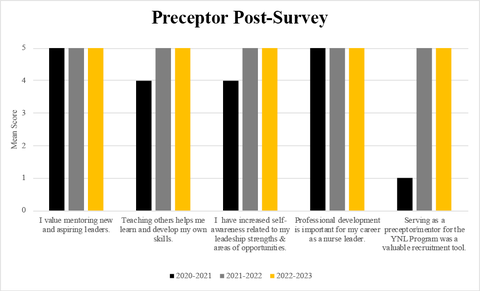
Five (62.5%) YNL program preceptors completed a post-survey (Figure 4). Overall, preceptors expressed satisfaction with the program in terms of professional development and joy in precepting pre-licensure students. One preceptor completed a survey from Cohort 1 so some of the lower scores can be attributed to the experience of 1 person. Changes were made in subsequent years to increase engagement and communication between PLs and preceptors. Of the preceptors who completed the post-survey, 100% said that they would recommend the YNL program to other nurse leaders.
Lessons Learned
The YNL program demonstrated the positive effect that a pre-licensure leadership program can have on undergraduate students partnered with practicing nurse leaders. Unanimous support and recommendation of the program to other students and practice leaders speaks to the benefits of a paired didactic and experiential learning opportunity to enhance nursing leadership knowledge and skills. As leadership priorities and topics shift over time, it will be important for PLs to be in sync with the ever-changing health care environment, and the academic environment that has re-affirmed the need for dedicated leadership development for entry-level professional nurses.
The second year of the YNL program was negatively impacted by a COVID-19 surge that shifted hospital operations and resource availability. While pandemic-related barriers may not exist moving forward, the demands and organizational priorities may impact future access to nurse leaders as program preceptors. Identifying opportunities to integrate a sustainable program is a key aspect of nursing leadership, so ongoing efforts continue strengthening the academic-practice partnership in place for this program.
One of the goals of the YNL program was to increase awareness of and interest in nursing leadership career paths. Future data collection should include information regarding the career progression for YNL participants. Additionally, information on whether students return to graduate school to study nursing leadership is of interest. The long-term impact of the program on career trajectory and leadership impact are still unknown. However, the hope is that the YNL program experience inspires participants to be leaders in all that they do as nurses.
This program highlighted an opportunity to connect nurse leaders with undergraduate students to excite their interest in nursing leadership as a specialty. An added benefit of fostering a mentee-mentorship relationship is the establishment of trust, which serves as a strong recruitment tool for a nurse residency program position on the leader’s team. We hope that nursing leadership continues to encourage, support, and facilitate mentorship opportunities for nurse leaders, as this program highlighted their appreciation and encouragement for the future generation of nursing leaders.
Acknowledgements
We appreciate the strong academic-practice partnership between the University of Iowa College of Nursing and the University of Iowa Hospitals & Clinics. Thank you to the students who participated in the YNL program and provided formative feedback. Last, but not least, thank you to the nurse leaders who dedicated the time and energy to mentor and preceptor our students. Without your commitment, engagement, and leadership, this program would not have the same impact and value.
References
- Joseph ML, Huber DL. Clinical leadership development and education for nurses: prospects and opportunities. J Healthc Leadersh. 2015;7:55-64.
- Pallesen KS, McCormack B, Kjerholt M, Borre LZ, Rosted E, Hølge-Hazelton B. An investigation of the level of burnout and resilience among hospital-based nurse managers after COVID 19 - A cross-sectional questionnaire-based study. J Nurs Manag. 2022;30(8):4107-4115.
- American Organization of Nursing Leadership (AONL). Longitudinal Nursing Leadership Insight Study Part 4: Nurse Leader’s Top Challenges and Areas for Needed Support, July 2020 to August 2022. 2022. https://www.aonl.org/system/files/media/file/2022/10/AONL%20Longitudinal%20Nursing%20Leadership%20Insight% 20Study%20Report%20L4%20Final.pdf. Accessed June 2, 2023.
- Dimino K, Learmonth AE, Fajardo CC. Nurse managers leading the way: Reenvisioning stress to maintain healthy work environments. Crit Care Nurse. 2021;41(5):52-58.
- American Association of Colleges of Nursing. The Essentials: Core competencies for professional nursing education. 2021. https://www.aacnnursing.org/Portals/42/AcademicNursing/pdf/Essentials-2021.pdf
- Cooke, M. Exploring strengths of prelicensure nursing students to build leadership potential. J. Nurs. Educ. 2021;46(6):e139-140.
- Joseph, ML, Phillips, BC, Edmondson, C, Godfrey, N, Liebig, D, Luparell, S, Weybrew, K. The nurse leader’s role: A conduit for professional identity formation and sustainability. Nurse Lead. 2021;19(1),27-32.
- Grossman S, Valiga TM. The New Leadership Challenge: Creating the Future of Nursing. F.A. Davis; 2021.
- Page A, Halcomb E, Sim J. The impact of nurse leadership education on clinical practice: An integrative review. J Nurs Manag. 2021;29(6):1385-1397.
- Kim HO, Lee I, Lee BS. Nursing leaders' perceptions of the state of nursing leadership and the need for nursing leadership education reform: A qualitative content analysis from South Korea. J Nurs Manag. 2022;30(7):2216-2226.
- Hughes, R, Meadows, MT, Begley, R. American organization for nursing leadership nurse leader core competencies: A framework reaching across the continuum and leadership levels. J Nurs Adm. 2022;52(12):629-631.
- Miles JM, Scott ES. A New Leadership Development Model for Nursing Education. J Prof Nurs. 2019;35(1):5-11.
- Godfrey N, Young E. Professional Identity. In: Giddens J, ed. Concepts for Nursing Practice. 3rd ed. Elsevier; 2020.
- American Association of Critical-Care Nurses. AACN standards for establishing and sustaining healthy work environments: a journey to excellence. Am J Crit Care. 2005;14(3):187-97.