View as pdf
A later version of this article appeared in Nurse Leader, Volume 21, Issue 6, December 2023.
Abstract
High turnover of unlicensed assistive personnel can have a significant fiscal impact on healthcare organizations. More importantly, the attrition rates set the groundwork for missed elements in patient care. Unprecedented employment challenges inspired one group of leaders to develop an innovative, cost-effective unit partner role to address turnover rates and support demanding workloads. The role enables flexibility, a nimble orientation structure, and university partnership. Consequently, this role affords nurses further opportunities to practice at the top of their licensure. Ultimately, fostering a supportive hiring process for healthcare students allows for ease of progression from entry-level to professional nurse.
In the immediate aftermath of the novel coronavirus pandemic, strained healthcare systems faced workforce shifts, increasing patient volumes, and high patient acuity. Many employees were retiring, leaving the workforce altogether, or seeking new opportunities, necessitating the reliance on temporary agency personnel to fill staffing gaps. Patients, who delayed seeking care during the pandemic months, were presented with worsening conditions and higher acuity of needs. The already strained workforce of unlicensed assistive personnel experienced high turnover rates and low volumes of qualified applicants. This transformed the landscape of post-pandemic healthcare and led a group of nurse leaders at the University of Iowa Hospitals & Clinics (UIHC), a large Midwest academic medical center to develop an innovative staffing solution to support depleted nursing resources while continuing to provide high-quality patient care.
At UIHC, the primary applicant pool of unlicensed assistive personnel, known as patient care technicians (PCT), is local University of Iowa students enrolled in nursing and healthcare programs. Post-pandemic, alongside many other organizations, UIHC experienced an increase in PCT turnover and recruitment challenges. High turnover rates of unlicensed assistive personnel can have a significant fiscal impact on healthcare organizations.1 In addition to financial costs, workforce strains contribute to missed elements of patient care, such as bathing, handwashing, ambulation, and oral care.2 To continue fulfilling the mission of high-quality patient care this necessitated adapting the approach of student recruitment and onboarding, ultimately leading to the creation of a new student job classification, the unit partner. The role of a unit partner provides “assistance” to the PCT and a much-needed set of hands at the front line where care is delivered.
An Innovative Way Forward
UIHC initially trialed the concept of a unit partner in 2017. The early pilot consisted of 8-unit partners divided between 2 units, a surgical intensive care unit and a monitored step-down neuroscience unit. Three lessons learned from the pre-pandemic pilot included: (1) importance of educating staff on the unit partner role, (2) identifying students’ knowledge level and training needs, and (3) determining unit partner orientation content to ensure students provide safe care.
With these lessons in hand, the UIHC leadership team reached out to their long-term partners, University of Iowa College of Nursing (UI-CON) deans, to collaborate on innovative strategies to reinvigorate the unit partner role in 2022. Pilot data collected from participants and unit staff laid the foundation for refining the role. To begin, 2 units were selected with engaged managers committed to providing the education needed for unit staff, while defining expectations for the unit partner role. The leadership team, consisting of UIHC unit managers, the divisional director, human resource representatives, Nursing Practice Leaders (NPL), and UI-CON academic deans, held regular meetings to refine the unit partner role and onboarding. At UIHC, NPLs lead nursing practice and patient care at the meso/macro system level and provide leadership for nursing practice or service lines based on systemic evaluation, evidence-based practice, and research, while assuring standard of care delivery and competency of staff across the units.3
Practice-Academic Collaboration
Collaborative discussions by the UIHC and UI-CON leadership teams led to refining the unit partner role and developing performance guidelines within state regulatory rules for unlicensed assistive personnel, orientation content, and flexible orientation schedules to onboard healthcare students.
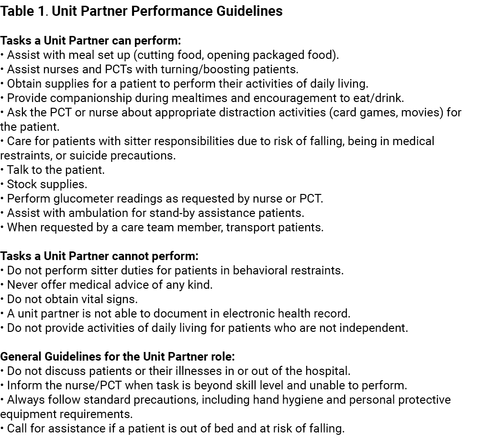
The UIHC leadership team completed a critical review of role expectations, unit needs, and state regulations, then developed the unit partner performance guidelines. Table 1 lists the performance recommendations.
Under direct supervision, unit partners perform routine tasks, participate in direct patient observation, and assist members of the care team.
The onboarding expectation was designed to enable flexible schedules for students, provide an introductory overview of expectations, and enable early relationships between the prospective hire and unit-level leadership. To meet competency and regulatory requirements, the UIHC leadership team developed the orientation content to include in-person didactic education, asynchronous online learning modules, and hands-on unit orientation. Table 2 outlines the orientation overview and progression of learning.
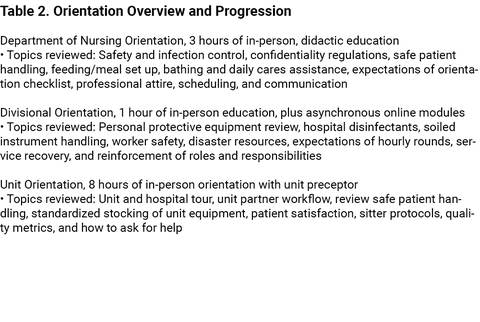
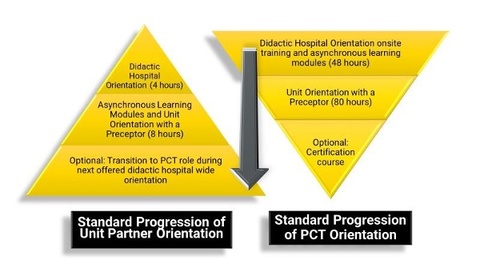
The team narrowed the didactic orientation content to 4 hours, improving efficiency for students. Comparatively, PCTs must commit to 40 hours of hospital orientation and are limited to onboarding during university breaks. A flexible orientation schedule is essential to recruiting and training students to the unit partner role throughout the academic year, thus 4-hour synchronous orientation sessions are offered morning, afternoon, and evening. After completion of didactic content, unit partners tour their assigned unit and meet nurse managers to discuss the 8-hour unit-based orientation schedule and role expectations. Figure 1 compares the standard progression of orientation for a PCT and a unit partner, demonstrating a reduction of 116 hours of initial orientation time.
The leadership team continued to collaborate throughout the pilot and modified content for prospective hiring groups. UI-CON academic deans and staff assisted in refining and dispersing unit partner advertising materials to all nursing students including first-year students and sophomores. In addition, they use the UIHC collaborative relationship and the unit partner role as a recruitment strategy for prospective nursing students, “come to the University of Iowa and flexible employment as a unit partner is available at UIHC.” All levels of nursing students share an appreciation of on-the-job learning to complement their nursing education. Nursing students commonly quickly progress from the unit partner to PCT role.
Unit Integration
Nursing staff buy-in was key to the successful integration and implementation of the new unit role. The unit partner role was curated to positively influence the team’s ability to deliver safe, high-quality, patient-centered care. The UIHC leadership team promoted the role as an “assistant to the PCT” to help spark intrinsic staff motivation, “Accepting this new role into my team will ultimately assist me in delivering quality care.” Staff meetings were held to brainstorm ways the unit partner could assist care teams. Clinical staff were invited to share feedback and suggestions beneficial to the unit integration.
The team began by standardizing the unit partner’s interview. In the candidate's interview unit leaders described their unit, the orientation process, and self-scheduling guidelines.
Unit leaders also reviewed the unit partner job description and explained the importance of being outgoing and self-motivated. A standardized interview template helped leaders deliver clear expectations to the new hires. In the unit partner’s orientation, the unit partner performance guidelines were reviewed. Unit partners were provided badge tags outlining patient care tasks they can and cannot perform. Nurse leaders empowered this highly engaged group of staff to speak up if they were uncomfortable with a delegated task or felt it was outside of their scope of practice. The leaders continued to promote role and performance guidelines throughout the transition and incorporation of unit partners into care teams.
Early Results
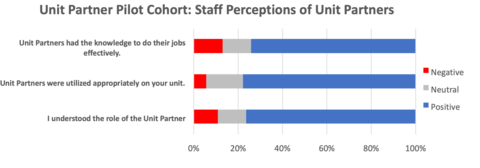
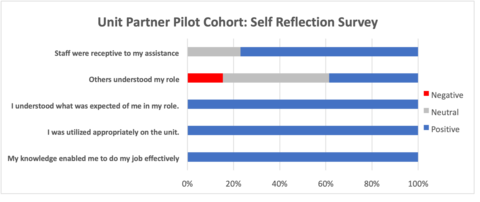
The pilot cohort was hired in the spring of 2022. Eighteen-unit partners were hired between two inpatient medical-surgical units. Three months after unveiling the new position, the unit partners and clinical staff were surveyed regarding their perceptions of the new role. The survey data was reviewed by the UIHC leadership team to help make decisions on the future direction and sustainability of the unit partner role. Overall, the survey data was positive and validated the belief that unit partners could be successfully onboarded and integrated into our care teams (see Figure 2).
The survey identified the largest opportunity for improvement was communication about the new role with the staff, as shown in Figure 3. The nurses and PCTs needed additional [and ongoing] information about the unit partner role—training content, appropriate tasks, and delegation opportunities.
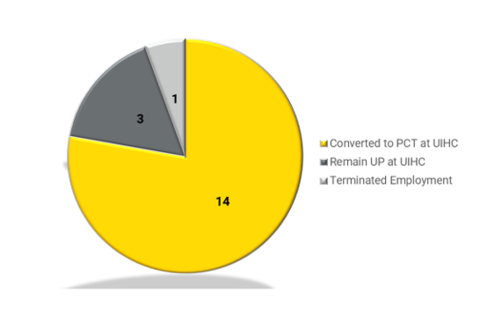
The UIHC leadership team reviewed employment data 3, 6, and 12 months after the unit partner hire date to understand the impact of the unit partner role on PCT recruitment and retention. Three months after hire, 10 of the initial unit partners converted to PCTs (56%), 7 remained in the unit partner role (39%), and one determined that it was not a suitable time in life to have a job (5%). Six months after hire, 4 additional unit partners completed the PCT orientation, while 3 remained unit partners. There were no employment changes between 6 and 12 months; the cohort ended with a first-year retention rate of 94.4%. One-year job classification outcomes are shown in Figure 4.
Growth and Expansion
The UIHC leadership team presented pilot data, lessons learned, and recommendations for expansion to the Chief Nurse Executive (CNE) and the nursing directors. UIHC CNE approved 120 new unit partner positions; nursing directors and nurse managers collaborated to determine target hire numbers based on unit size and staffing vacancies (nurse and PCT). Human Resource recruiters and members of the leadership team attended fall semester University sponsored events such as College of Nursing Welcome Social, the President’s block party, and a formal student job fair to answer questions and raise awareness of available healthcare employment opportunities. In the first semester post-pilot, UIHC recruiters connected with over two hundred interested students in these informal settings. Fifteen units across all divisions (medical-surgical, intensive care, behavioral health, and children’s/women’s) interviewed and hired unit partners, filling 116 unit partner positions.
Nurse managers from the pilot units shared their experiences and best practices with the other nurse managers hiring and onboarding unit partners for the first time. Nursing practice leaders modified the orientation plan based on survey data and recommendations from the UIHC leadership team. After orientation and integration into the unit, unit partners can transition into a PCT position during academic breaks. Unforeseen benefits of this transition included the ease of orienting unit partners into an expanded PCT role and a reduction in the length of orientation. Unit partners shared how the familiarity of the team and inpatient care area reduced anxiety about expanding role responsibilities. PCT orientation was reduced overall by 12 hours since unit partners fulfilled many of these overlapping competencies and qualifications during initial orientation. Some units cited a reduction in unit-based orientation hours due to robust performance in the PCT role and familiarity with the patients, unit, equipment, and staff. There is potential for future orientation reduction as the leadership team reviews the unit partner program.
Lessons Learned
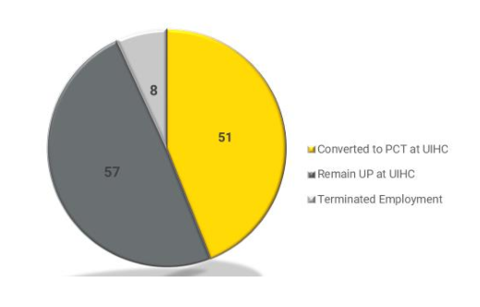
An additional benefit of the collaborative practice-academic partnership between UIHC and UI-CON is the ease of connecting university students to the hospital recruitment team. This collaboration supports student learners, who are seeking healthcare experiences to identify open positions at the affiliated medical center. As student learners progress through nursing and healthcare programs, UIHC provides opportunities for professional development and career growth. The unit partner role serves as a pipeline for hiring and onboarding PCTs. As PCTs complete nursing programs, the leadership team will continue to monitor the unit partner cohort groups for anticipative progression into a nursing position upon graduation. The employment outcomes for the 116 unit partners hired in the Fall semester of 2022 appear in Figure 5. Ninety three percent of unit partners remain employed at UIHC six months after hire; almost half of the group transitioned into a PCT position. For those unit partners choosing to remain in their role or those enrolled in non-nursing related programs, the attained direct patient care hours offer invaluable opportunities to interact with patients and families and develop the soft skills essential to providing compassionate, connected care.
Both healthcare students and nurse leaders enjoy the flexible schedule and nimble orientation of the unit partner role. This unique position allows student employees to schedule hours based on their academic schedules. A suggested 8 hours per week can be fulfilled through 2, 4, 8, or 12 hour shifts, depending upon the availability of the student. During the initial pilot, unit partners worked an average of 9 hours per week and shared positive feedback on the ease of incorporating the flexible hours of employment into their academic schedules. Nurse leaders appreciate the additional staff present on the unit, often during off-shifts, evenings, and weekends to support nurses and PCTs with tasks and address patient needs. Unit partners provide focused attention to the care and small needs of the patients, freeing up the registered nursing staff to practice at the top of their license and training while facilitating a team-centric approach to patient care.
Conclusion
The transformed landscape of post-pandemic healthcare led a group of UIHC leaders to develop an innovative staffing solution to support depleted nursing resources while continuing to provide high-quality patient care. The creation of the unit partner role is a cost-effective solution that supports the demanding workload for nurses and PCTs and allows staff to practice at the top of their licensure and training. Additionally, the role flexibility, nimble orientation structure, and university partnership foster a supportive hiring process that grows with the student learner and allows for ease of professional progression into a PCT role and eventual nursing position. The UIHC leadership team recognized the need to develop creative staffing solutions to continually provide excellence in patient care while supporting staff and students.
Acknowledgements
Thank you to the leadership at University of Iowa Hospitals & Clinics, University of Iowa College of Nursing, and all who helped make this innovative idea a reality. The authors would specifically like to thank Dr. Julie Zerwic (Dean College of Nursing), Dr. Sandra Daack-Hirsch (Executive Associate Dean), Kyle Fountain (nursing recruitment), Kelly Petrulevich (nurse manager), and early adopters on 4JPP and 6RC who embraced the unit partner role and integrated the concept into practice.
References
- Gion T, Abitz T. An approach to recruitment and retention of certified nursing assistants using innovation and collaboration. Journal of Nursing Administration. 2019; 47(7/8): 354-358.
- Orique SB, Patty CM, Woods E. Missed nursing care and unit-level nurse workload in the acute and post-acute settings. Journal of Nursing Care Quality. 2016; 31(1): 84-89.
- University Job Classification; University of Iowa Hospitals & Clinics; 2023; Accessed June 30, 2023