View as pdf
A later version of this article appeared in Nurse Leader, Volume 21, Issue 6, December 2023.
Abstract
Technology, such as clinical decision support, can play a role in supporting nurses’ decision making, but understanding the complexity and current challenges in nurse decision-making is needed to guide the implementation of technology interventions focused on supporting effective decision-making in practice and leadership. The purpose of this article is to discuss decision-making and information needs among nurses across roles and explain how technology and implementation science approaches can complement effective decision-making interventions.
Across settings and nursing roles, effective decision-making is fundamental to excellent nursing and patient care. For example, nurses in patient care roles often spend more time with patients than any other health discipline and frequently need to make decisions about when to inform the health care team with changes in a patient’s condition. Nurses in leadership roles must make a wide range of managerial decisions concerning nurse staffing, human resources, and which clinical technologies to advocate for the support direct care nurses’ decision-making. Factors such as increasing patient acuity, escalating evidence base, and global pandemics have led to increased complexity in nurse decision-making across roles. Technology can play a role in supporting nurses’ decision making, but understanding the complexity and current challenges in nurse decision-making is needed to guide the implementation of technology interventions focused on supporting effective decision-making in practice and leadership. The purpose of this article is to discuss decision-making and information needs among nurses across roles and explain how technology and implementation science approaches can complement effective decision-making interventions.
Decision-making Across Nursing
Decision-making, or executing a choice among options, is an essential process in nursing and numerous theories and models have been developed to describe and study nurse decision-making.1-3 Approaches to decision-making can be broadly categorized as rational, using logical steps or rule-based thinking to determine the best option, or intuitive, which describes using instinct or subconscious pattern recognition to make a choice.4 Over time, thinking has transformed from viewing nurse decision-making as primarily a rational process, to a process that is influenced by real-world demands, such as needing to make decisions with limited information, changing conditions, interruptions, and/or time pressure.5,6 In these situations, experienced nurses rapidly apply insight from previous experiences to make decisions.7,8 Given the variation in how decisions are made and real-world demands that nurses and leaders are faced with, a one-size-fits-all approach may not be useful when developing and implementing nurse decision-making interventions.
Information is a fundamental component of the decision-making process and is generated from diverse sources. Digital technologies (e.g., clinical decision support, telehealth, monitoring systems, artificial intelligence) can provide important new sources of information and address limitations to existing information sources, such as organizing EHR data to efficiently identify a patient’s risk for clinical deterioration. However, technologies that fail to adequately address information needs, or are difficult to use, will have limited adoption. Understanding the types of information nurses need in direct care and leadership roles, what information is available, and limitations to existing information sources is needed to evaluate interventions to support decision-making.
Technologic Considerations for Supporting Direct Care Nurses’ Information Needs
Nurses need timely, patient-specific clinical information to provide care. The electronic health record (EHR) is the primary source of patient data, however substantial documentation demands have significantly impacted nurse workload and workflows for finding relevant information. Studies estimate that nurses spend 35 to 41% of their time in the EHR documenting and reviewing patient information.9,10 While nurses generate large amounts of data in the EHR, documenting an average of 631-875 flowsheet data points and spending an average of 21 minutes documenting notes per shift, there are significant challenges with organizing and synthesizing patient data.11,12
An integrative review of EHR’s impact on nurses’ cognitive work identified the following limitations to meeting nurse information needs in the EHR: developing an overview of the patient’s history, current status, and plan; synthesizing information using EHR-generated reports to support information needs during a shift and at handoff; and achieving shared understanding of patient goals and care coordination.13 Similar needs were found by Keenan et al. over a decade ago including the need for a centralized overview of patients accessible to all members of the healthcare team and effective technology to support nurse to nurse change of shift handoffs.14 Given these challenges, work in two key areas – reducing documentation burden in the EHR and incorporating nurse information needs into EHR redesign are critical to support direct care nurse work.
Another critical area is related to nurses’ expectation to incorporate research into decision-making. This is commonly referred to as evidence-based practice: applying the best available evidence along with patient preferences in making clinical decisions and is a foundation of high-quality nursing care.15 However, there is a persistent gap of 15 to 17 years between current best evidence and daily practice.16,17 Studies of information needs and information use for evidence-based practice offer additional perspectives for understanding barriers to routinely using evidence in practice. Findings over the past 15 years indicate that nurses routinely seek out information from colleagues since they share clinical context and are accessible.18,19 However, information shared by colleagues may be outdated or inaccurate when technology-based tools, such as clinical decision support, can provide nurses with up to date accurate information during a time that integrates well with nurses decision making workflow.
Technologic Considerations for Supporting Nurse Leaders’ Information Needs
Nurse leaders across roles and settings must integrate patient and organizational data to optimize patient outcomes. Information needs vary by timing of decision. Nurse managers describe short-term information needs about patients related to throughput and staffing needs and long-term information needs focused on meeting organizational priorities, such as quality improvement initiatives and nurse retention.20, 21 Whereas short-term information was commonly reported to come from the EHR and situational awareness, or understanding of the local environment, long-term information needs require leaders to search for information across sources. A recent review of nursing management information systems found that nursing leaders use information systems to manage human resources, determine nursing workload (nurse to patient ratio) and control costs.22 These systems are largely based on two sources of data: patient classification measures and hospital resource measurement. The authors did not find a central database or decision support tool to support the work of nurse leaders, suggesting a critical need for new technology to address this gap.
In addition to their own information needs, nurse managers play a critical role in advocating for the information needs of the direct care nurses. For example, in the United States there are an increasing number of mandates and digital technologies related to care quality issues such as central line infection and hospital acquired pressure ulcer prevention. Nurse leaders must appraise digital technologies to determine whether the technology supports the direct care nurses’ information needs, ensure that it is easy to use and does not add to nursing workload as well as providing a return on investment.
A Role for Clinical Decision Support
One technology-based intervention to assist nurses in complex in decision-making processes is clinical decision support (CDS) systems. CDS systems are computer-based tools to organize person-specific data and knowledge for clinicians and patients to improve the quality and safety of health care.23 CDS is delivered in a variety of formats, such as through order sets, documentation templates, computerized alerts, dashboards, and visualizations, which may be integrated in electronic health record (EHR) systems or exist as applications or technologies outside the EHR. In general, CDS is composed of three key parts.24
- Data management: clinical data and decision rules or logic. Decision rules or logic may be developed using literature and current practice (knowledge-based) or artificial intelligence (non-knowledge-based).
- Processing: applies the knowledge or algorithms with patient data
- User interface: the part of the system that communicates a recommendation and is the point the user interacts with (e.g., computer display, mouse).
Guiding principles for developing effective CDS are known as the CDS Five Rights, and state that CDS should communicate the right information, to the right person, in the right format, through the correct channel at the right time in the workflow.25 These principles provide a valuable framework for nurse leaders to consider in evaluating potential CDS tools.
CDS tools support information management, which is an increasing need in healthcare given the large volumes of clinical, administrative and research data that is generated. Therefore, tools which filter relevant patient data and apply logic to determine a recommendation are needed. However, fewer CDS tools have been developed for nurses than have been for physicians and other members of the health care team.26
Current Challenges and Opportunities in Nursing Clinical Support
Recognizing the opportunities for CDS to supporting decision-making must be balanced with the reality that gaps in developing and using CDS exist in nursing. A recent review of CDS tools across multiple disciplines found that only two-thirds of clinicians’ report using available CDS.27 While understanding of CDS usage specifically among nurses is limited, several nurse, patient, organization, and technology factors have been identified to influence nurses’ use of CDS.28 Given these challenges, the role of implementation science is emerging as an important approach to inform future CDS design and use.29
Implementation Science
Implementation science centers on how evidence-based practices are adopted and sustained across specific settings.30 Whereas evidence-based practice describes what recommendation should be used, implementation science focuses on how to best help people consistently do a particular recommendation in their work environment.31 Implementation science frameworks provide guidance for understanding key components of implementation, such as describing the implementation process, identifying barriers and facilitators to implementation, or conducting an implementation evaluation.32 Implementation strategies and context important concepts across most implementation science frameworks. Implementation strategies describe the specific interventions chosen to facilitate change. For example, the Iowa Implementation Model for Sustainability Framework provides an organized approach for selecting an implementation strategy based upon phases of implementation.33 For example, after nurses have obtained knowledge about a practice change, audit and feedback may be one implementation strategy to promote adoption. Related, is the concept of context, or the unique local factors (e.g., unit culture, work environment, resources) that influence how or why implementation is achieved.34 In partnership with implementation scientists, nurse leaders can identify unique barriers and facilitators to implementation in the local environment and then match the needs to implementation strategies.
Leveraging User-Centered Design
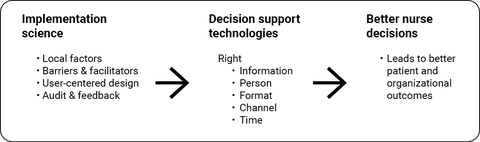
Considering the unique needs of users, or user-centered design, is a concept central to implementation science and CDS design (Figure 1). The goal of user-centered design is to make interventions “useable and useful” by focusing on user needs throughout the design and development process.35 Implementation science and user-centered design use a variety approaches to obtain end-user input, which may include, workflow mapping, participatory design, rapid prototyping, and usability testing.36, 37 However, methods to engage nurses early in CDS design and implementation are inconsistently applied.
Nurse leaders are in a key position to advocate for greater involvement of nurses, early and throughout the process of developing and implementing CDS. This may include developing processes for nurses to provide feedback about information needs in their settings, workflow considerations, and opportunities to test and refine CDS prototypes. Greater involvement of nursing informatics within organizations and including opportunities for nurses to receive training in implementation science and user-centered design are additional strategies to support integration of these concepts in CDS design and use.38-40 An organizational culture that supports nurse information needs by considering both the types of CDS that nurses need and how CDS will be used in daily practice is critical, especially as new technologies are developed and CDS becomes more complex.
Conclusion
Nurses and nurse leaders need to make numerous decisions in highly complex work environments. CDS has an expanding potential to augment decision-making across roles by providing nurses with meaningful, person-specific information in a usable format to positively impact care and outcomes. Nurses that will be the eventual user of the CDS need to be involved early and throughout CDS development to ensure that CDS tools are usable, useful, align with workflow as a part of routine work. Implementation scientists, who understand the local context, are needed to design and test strategies for using CDS, both in specific settings and diffusing CDS use across settings. Approaches which consider both how CDS is designed for nurse users and how CDS is used and implemented across health systems is needed to support effective decision-making for driving change in nursing practice and leadership settings.
References
- Lauri S, Salanterä S. Decision-making models in different fields of nursing. Res Nurs Health. Oct 1998;21(5):443-52. doi:10.1002/(sici)1098-240x(199810)21:5<443::aid-nur7>3.0.co;2-n
- Tanner CA. Thinking like a nurse: a research-based model of clinical judgment in nursing. J Nurs Educ. Jun 2006;45(6):204-11.
- Johansen ML, O'Brien JL. Decision making in nursing practice: a concept analysis. Nurs Forum. Jan-Mar 2016;51(1):40-8. doi:10.1111/nuf.12119
- Hamm RM. Clinical intuition and clinical analysis: expertise and cognitive continuum. In: Dowie JE, A, ed. Professional judgment : a reader in clinical decision making. Cambridge University Press; 1988:78-105.
- Nibbelink CW, Brewer BB. Decision-making in nursing practice: An integrative literature review. J Clin Nurs. Mar 2018;27(5-6):917-928. doi:10.1111/jocn.14151
- Thompson C, Dalgleish L, Bucknall T, et al. The effects of time pressure and experience on nurses' risk assessment decisions: a signal detection analysis. Nurs Res. Sep-Oct 2008;57(5):302-11. doi:10.1097/01.NNR.0000313504.37970.f9
- Benner P, Tanner C. How expert nurses use intuition. AJN. 1987;87(1):23-34.
- Melin-Johansson C, Palmqvist R, Rönnberg L. Clinical intuition in the nursing process and decision-making-A mixed-studies review. J Clin Nurs. Dec 2017;26(23-24):3936-3949. doi:10.1111/jocn.13814
- Schenk E, Schleyer R, Jones CR, Fincham S, Daratha KB, Monsen KA. Time motion analysis of nursing work in ICU, telemetry and medical-surgical units. J Nurs Manag. Nov 2017;25(8):640-646. doi:10.1111/jonm.12502
- Yen PY, Kellye M, Lopetegui M, et al. Nurses' time allocation and multitasking of nursing activities: a time motion study. AMIA Annu Symp Proc. 2018;2018:1137-1146.
- Hripcsak G, Vawdrey DK, Fred MR, Bostwick SB. Use of electronic clinical documentation: time spent and team interactions. JAMIA. Mar-Apr 2011;18(2):112-7. doi:10.1136/jamia.2010.008441
- Collins S, Couture B, Kang MJ, et al. Quantifying and visualizing nursing flowsheet documentation burden in acute and critical care. AMIA Annu Symp Proc. 2018;2018:348-357.
- Wisner K, Lyndon A, Chesla CA. The electronic health record’s impact on nurses’ cognitive work: An integrative review. Int J Nurs Stud. 2019/06/01/ 2019;94:74-84. doi:https://doi.org/10.1016/j.ijnurstu.2019.03.003
- Keenan G, Yakel E, Dunn Lopez K, Tschannen D, Ford YB. Challenges to nurses' efforts of retrieving, documenting, and communicating patient care information. JAMIA. Mar-Apr 2013;20(2):245-51. doi:10.1136/amiajnl-2012-000894
- Melnyk BM, Fineout-Overholt E. Evidence-based practice in nursing & healthcare: A guide to best practice. Lippincott Williams & Wilkins; 2022.
- Balas EA, Boren SA. Managing clinical knowledge for health care improvement. Yearb Med Inform. 2000;9(01):65-70.
- Khan S, Chambers D, Neta G. Revisiting time to translation: implementation of evidence-based practices (EBPs) in cancer control. Cancer Causes Control. 2021/03/01 2021;32(3):221-230. doi:10.1007/s10552-020-01376-z
- Clarke MA, Belden JL, Koopman RJ, et al. Information needs and information-seeking behaviour analysis of primary care physicians and nurses: a literature review. Health Info Libr J. Sep 2013;30(3):178-90. doi:10.1111/hir.12036
- Fossum M, Opsal A, Ehrenberg A. Nurses' sources of information to inform clinical practice: An integrative review to guide evidence-based practice. Worldviews Evid Based Nurs. Oct 2022;19(5):372-379. doi:10.1111/wvn.12569
- Peltonen LM, Siirala E, Junttila K, et al. Information needs in day-to-day operations management in hospital units: A cross-sectional national survey. J Nurs Manag. Mar 2019;27(2):233-244. doi:10.1111/jonm.12700
- Siirala E, Salanterä S, Lundgrén-Laine H, Peltonen LM, Engblom J, Junttila K. Identifying nurse managers' essential information needs in daily unit operation in perioperative settings. Nurs Open. May 2020;7(3):793-803. doi:10.1002/nop2.454
- Fathian A, Emami H, Moghaddasi H, Kazemi A, Rabiei R. Features of nursing management information systems: A systematic review. Biomed J. 2019;21(2):15773-15781.
- Teich JM, Osheroff JA, Pifer EA, Sittig DF, Jenders RA, Panel TCER. Clinical decision support in electronic prescribing: recommendations and an action plan: report of the joint clinical decision support workgroup. JAMIA. 2005;12(4):365-376. doi:10.1197/jamia.M1822
- Sutton RT, Pincock D, Baumgart DC, Sadowski DC, Fedorak RN, Kroeker KI. An overview of clinical decision support systems: benefits, risks, and strategies for success. NPJ Digit Med. 2020;3:17. doi:10.1038/s41746-020-0221-y
- Osheroff JA. Improving medication use and outcomes with clinical decision support:: a step by step guide. HIMSS; 2009.
- Dunn Lopez K, Gephart SM, Raszewski R, Sousa V, Shehorn LE, Abraham J. Integrative review of clinical decision support for registered nurses in acute care settings. JAMIA. Mar 1 2017;24(2):441-450. doi:10.1093/jamia/ocw084
- Kouri A, Yamada J, Lam Shin Cheung J, Van de Velde S, Gupta S. Do providers use computerized clinical decision support systems? A systematic review and meta-regression of clinical decision support uptake. Implement Sci. Mar 10 2022;17(1):21. doi:10.1186/s13012-022-01199-3
- Piscotty R, Kalisch B. Nurses' use of clinical decision support: a literature review. Comput Inform Nurs. Dec 2014;32(12):562-8. doi:10.1097/cin.0000000000000110
- Trinkley KE, Kroehl ME, Kahn MG, et al. Applying clinical decision support design best practices with the practical robust implementation and sustainability model versus reliance on commercially available clinical decision support tools: randomized controlled trial. JMIR Med Inform. Mar 22 2021;9(3):e24359. doi:10.2196/24359
- Brownson RC, Colditz GA, Proctor EK. Dissemination and implementation research in health: translating science to practice. Oxford University Press; 2018.
- Curran GM. Implementation science made too simple: a teaching tool. Implement Sci Commun. 2020;1:27. doi:10.1186/s43058-020-00001-z
- Nilsen P. Making sense of implementation theories, models and frameworks. Implement Sci. Apr 21 2015;10:53. doi:10.1186/s13012-015-0242-0
- Cullen L, Hanrahan K, Edmonds SW, Reisinger HS, Wagner M. Iowa implementation for sustainability framework. Implement Sci. Jan 4 2022;17(1):1. doi:10.1186/s13012-021-01157-5
- Nilsen P, Bernhardsson S. Context matters in implementation science: a scoping review of determinant frameworks that describe contextual determinants for implementation outcomes. BMC Health Serv Res. Mar 25 2019;19(1):189. doi:10.1186/s12913-019-4015-3
- Vaisson G, Provencher T, Dugas M, et al. User involvement in the design and development of patient decision aids and other personal health tools: a systematic review. Med Decis Making. Apr 2021;41(3):261-274. doi:10.1177/0272989x20984134
- Nielsen J. The usability engineering lifecycle. In: Nielsen J, ed. Usability Engineering. Academic Press; 1993:88-90.
- Dopp AR, Parisi KE, Munson SA, Lyon AR. Aligning implementation and user-centered design strategies to enhance the impact of health services: results from a concept mapping study. Implement Sci Commun. 2020/02/26 2020;1(1):17. doi:10.1186/s43058-020-00020-w
- Chipps E, Tucker S, Labardee R, et al. The Impact of the Electronic health record on moving new evidence-based nursing practices forward. Worldviews Evid Based Nurs. Apr 2020;17(2):136-143. doi:10.1111/wvn.12435
- Boehm LM, Stolldorf DP, Jeffery AD. Implementation science training and resources for nurses and nurse scientists. J Nurs Scholarsh. Jan 2020;52(1):47-54. doi:10.1111/jnu.12510
- Risling TL, Risling DE. Advancing nursing participation in user-centred design. J Res Nurs. May 2020;25(3):226-238. doi:10.1177/1744987120913590